LEARNING ON THE GO
Sara Temkit, 1T7
1. What Future Pharmacists Should Know About Beta-Blockers
Beta-blockers (BBs) were originally developed to counteract the adverse effects of adrenaline on the heart.
They have been shown to prevent mortality and morbidity in patients with cardiac disease, and have a compelling
indication in patients with angina, atrial fibrillation, and post-MI. Possible indications for BBs include stable
heart failure. Interestingly, BBs are also a first-line option for the treatment of hypertension in women of childbearing
potential due to the concern of fetal renal abnormalities with the use of alternatives such as ACE inhibitors or ARBs. (1)
As pharmacists, we need to understand the pharmacology of BBs. There are actually three beta-receptors, and it is the beta-1
adrenergic receptor that is mostly located in the heart. Beta-1 receptor activation often leads to an increase in heart
rate (positive inotropic effect) and myocardial contraction (positive chronotropic effect). In contrast, the beta-2 adrenergic
receptor is mostly located in bronchial and vascular smooth muscle and Beta-2-receptor activation can lead to broncho- and vasodilation. (2)
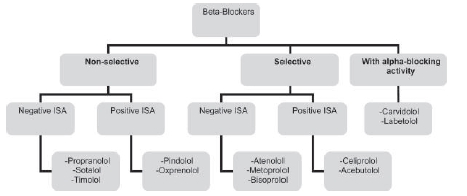
The first-generation non-selective BBs (i.e. propranolol, nadolol, timolol, and sotalol) act on both beta-1 and beta-2 adrenergic
receptors. The blockade of the beta-1 receptor allows a reduction in heart rate and contractility, and blockade of the beta-2 receptors results in smooth muscle contraction and bronchospasm. The blockade of the beta-2 receptor can also lead to the constriction of blood vessels supplying skeletal muscle, exacerbating Reynaud's phenomenon (syndrome of cold hands and feet). (2)
In contrast to the first-generation agents, the second-generation agents are selective BBs (i.e. atenolol, bisoprolol, metoprolol), and they selectively act at the beta-1 receptor of the heart. The second-generation agents are preferred in patients with lung disease (i.e. asthma or COPD), who are more prone to side effects caused by non-selective agents (i.e. bronchospasm). However, it is important to note that cardioselectivity of the second-generation agents is lost when higher doses are used. (2)
The third-generation BBs have unique vasodilatory properties. They can be selective (i.e. nebivolol) or non-selective (i.e. carvidolol and labetolol). They cause vasodilation of peripheral vasculature via additional alpha-adrenergic blockade of vascular smooth muscle receptors. Some beta-blockers also mediate vasodilation via B2-intrinsic sympathomimetic activity (ISA). These beta-blockers are partial agonists of the beta-receptor (having the capacity to both block and stimulate beta-receptor activity). Beta-blockers with ISA cause less bradycardia and less coolness in the extremities. However, agents with ISA are not often used as they have not been proven to be beneficial in patients with angina, atrial fibrillation or post-MI. (2)
All beta-blockers can cause bradycardia and fatigue due to reduced cardiac output. However, non-selective beta-blockers are more likely to induce tiredness upon exertion due to reduced blood flow to skeletal muscle. All beta-blockers can cause reduced sympathetic flow in the Central Nervous System (CNS), resulting in vivid dreams, nightmares, and rarely hallucinations. Lipid-soluble beta-blockers are the greatest offenders as they have greater penetration into the CNS. All beta-blockers should also be used with caution in patients with diabetes due to the masking of symptoms of hypoglycemia (i.e. tachycardia).
Lastly, when discontinuing beta-blockers, ALWAYS use a taper. Abrupt withdrawal of BBs can lead to "beta-blocker rebound phenomenon" including tachycardia, rise in blood pressure, increased angina attacks, and worsening of heart failure symptoms. This rebound phenomenon is likely due to increased beta-adrenergic receptor responsiveness (increased sensitivity to catecholamines or rebound adrenergic hypersensitivity). Regardless of whether you choose to work in the hospital or the community, patients on high-dose BBs should be warned of the consequences of abrupt BB withdrawal. (3)
Sources:
Sources:
1.British Hypertension Society. (Dec, 2008). Retrieved from http://www.bhsoc.org/pdfs/therapeutics/Beta-adrenoceptor%20Antagonists%20(Beta-Blockers).pdf.
2.Albouaini, K., Andron, M., Alahmar, A., & Egred, M. (2007). Beta-blockers use in patients with chronic obstructive pulmonary disease and concomitant cardiovascular conditions. International journal of chronic obstructive pulmonary disease, 2(4), 535.
3.Koracevic, G. (2011). Significance of "beta blocker rebound phenomenon" and new suggestions how to avoid it. In Proceedings of the World Medical Conference, WSEAS (26-28 September 2011, Prague, Czech Republic), Prague (pp. 79-84)
Test Your Knowledge: Choosing the Right Beta-Blocker for Your Patient!
1.Which beta-blocker would you use for a patient with mild-moderate asthma or COPD?
Answer: A cardioselective beta-blocker (i.e. atenolol, metoprolol, bisoprolol)
2.Which beta-blocker would you use for a patient with severe asthma or COPD?
Answer: All beta-blockers are contraindicated in patients with severe asthma or COPD, as even the cardioselective beta-blockers lose their selectivity at higher doses.
3.Which beta-blocker would you use for a patient with insulin-dependent diabetes?
Answer: All beta-blockers can mask the symptoms of hypoglycemia (i.e. tachycardia). So, beta-blockers are only to be used in patients with diabetes and a compelling indication (i.e. coronary artery disease). If beta-blockers must be used, cardioselective beta-blockers are preferred, as they do not exacerbate hypoglycemia. Non-selective BBs inhibit beta-2-receptors in the liver, interfering with glycogenolysis and restoration of blood glucose levels.
4.Which beta-blocker would you use for a pregnant hypertensive patient with Reynaud's disease (increased coolness at extremities)?
Hint: The fact that the patient is pregnant should not affect your choice of beta-blocker.
Answer: Beta-blockers are second-line agents in patients with hypertension as they do not prevent mortality in this patient population. However, beta-blockers are first-line in pregnant, hypertensive patients due to lower risk of fetal morphological defects. In this particular patient with Reynaud's disease, a third-generation beta-blocker or a beta-blocker with ISA may be preferred due to vasodilatory activity (and reduced coolness at extremities).